Exams
Step 1: Preliminary Testing
Autorefractor
A friendly technician will start your examination by getting an estimation of prescription with an automated refractor, the Zeiss i.Profiler®plus. The i.Profiler®plus not only provides you a better prescription, it also gives you access to an optimized individualized lens solution with i.Scription® technology that calculates a prescription to 1/100th of a diopter for improved color and contrast vision as well as improved night vision.
Marco TRS 5100 (pictured left)
The Marco TRS-5100® replaces the manual refractor and allows the doctor to perform a more accurate, reliable, and comfortable prescription check for patients. Come experience a faster, more modern eye exam.

Eye Pressure
We then measure your eye pressure with a non-contact tonometer that blows a small gentle puff of air into your eyes. We use your eye pressure measurements as a factor to determine if you might be at risk for glaucoma.
Corneal Specular Microscope
Next we take a specular microscope scan of your cornea. We check the back side of the cornea, the corneal endothelium, as an indication of how healthy your cornea is to ensure that healthy contact lens wear can occur. We also screen the corneal endothelium to ensure that there are no corneal dystrophies or degenerations.

Optomap Retinal Examination
Last, we run the Optomap Retinal Scan. Early signs of disease can be present in the periphery of your retina and remain undetected for a long time when using traditional methods. The Optomap exam is fast, painless, and comfortable. Nothing touches your eye at any time. It is suitable for the whole family. To have the exam, you simply look into the device one eye at a time (like looking through a keyhole) and you will see a comfortable flash of light to let you know the image of your retina has been taken.
Under normal circumstances, dilation is no longer necessary when you do the Optomap exam and it only costs $39. The capture takes less than a second. Images are available immediately for review. You can see your own retina. You see exactly what your eye care practitioner sees – even in a 3D animation.
Step 2: Exam Room Workup
History
Your technician will make sure to take a complete and thorough medical and ocular history. We will want to know who your medical doctor is as well as all you pertinent medical information. Important things such as your medications and what you are allergic to will be great information to provide.
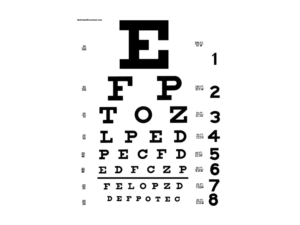
Visual Activity
Next we will check to see how well you can see. We will check your vision with and without visual correction. We ask that you bring all forms of vision correction that you have including contact lenses, glasses, computer glasses, reading glasses, and your sunglasses. Even bringing in old prescriptions or labels of previous contact lenses can be helpful to bring.
The standard for clear vision is 20/20. It means that you, the subject, can see at 20 feet what a reference person with “good” vision can see at 20 feet. 20/40 means you can see at 20 feet what the reference person can see at 40 feet. A driver’s license will have a vision correction restriction if either eye has 20/40 or worse vision.
If your vision is less than 20/20 in either eye or in both eyes, our job is figure out why. Glasses or contact lens can typically correct the most common reasons vision is below 20/20. If vision is less than 20/20 with correction, then we are looking for a medical explanation, such as a cloudy cornea, a cataract, or a retinal problem.
Step 3: Eye Doctor Eye Examination

Refraction
Here you will meet your eye doctor who will start the process of determining your vision correction. We will check for reasons why you might see blurry.
Myopia – Often referred to as “nearsighted” in which you have more trouble seeing things far away in the distance.
Hyperopia – Often referred to as “farsighted” in which you have more trouble seeing things at near range.
Astigmatism – When there is an uneven curvature in your eye that causes you to see things distorted at a certain angle. This can make you see blurry both at far and near ranges.
Presbyopia – When there is a loss of ability to focus up close. This happens naturally with time. Typically in the 40’s is when a patient first notices no longer being able to effectively see at near range due to the loss of elasticity in the crystalline lens of the eye.
Prescription
Your eye doctor will carefully explain the results of your refraction and start working with you to formulate what vision corrections are ideal. Visual correction options include glasses, contact lenses, and surgical options such as LASIK. Many patients elect to have both contact lens and glasses options so that they have different choices depending on what they are doing at a particular time.
People often say they don’t come in for an eye exam because their vision is “fine.” Unfortunately, there are several serious eye diseases like glaucoma and macular degeneration that can take away your vision even while you feel that you are seeing fine. Even if you have no risk factors it may be a good time to have a baseline eye exam to ensure that your eyes are healthy.
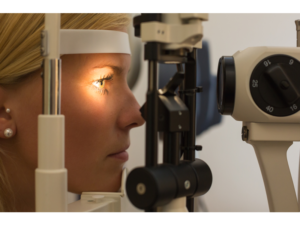

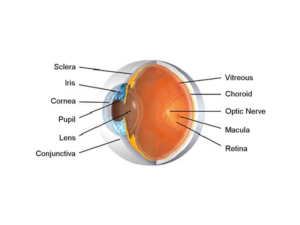
Microscope Exam of the Front of the Eye
A specialized “slit lamp” microscope is used to examine the fine details of the eye. We check the white part of the eye, the sclera, as well as the clear covering over the white part of the eye called the conjunctiva. Next, we’ll check the cornea, which is the clear window that covers the colored part of the eye. The cornea can become cloudy which will affect how well you see. We’ll determine whether there are any signs of an eye infection, ocular allergies, dry eyes or any corneal dystrophy.
As we start examining further into the eye, we will evaluate the iris which is the colored ring surrounding the dark pupil. Like the diaphragm of a camera, the pupil regulates the amount of light entering the eye by changing size.
The next structure we look at in the eyes is the crystalline lens. The lens changes shape and moves slightly forward to help focus up close. Over time, the lens gets less elastic and which can lead to our loss of ability to see at near. In everyone’s life, the lens becomes increasingly hazy and tinted in color. When the lens becomes cloudy we call it a cataract. When the cataract gets mature and vision becomes significantly reduced, we can make the timely referral to see if a cataract surgery is appropriate. Some things that are associated with accelerated cataract development are extended UV exposure, diabetes, trauma, and steroid (prednisone) use.

Exam of the Back of the Eye
The eye is an inflated hollow structure like a basketball. The large space behind the iris and lens is filled with a clear jelly-like material called vitreous. The vitreous cavity occupies the back 2/3 of the eye. Over time opacities gradually accumulate in the vitreous which cast shadows we see as vitreous floaters. Besides accumulation of the floaters, the vitreous gradually shrinks which causes it to pull on the places where it is attached to the retina. This pulling can mechanically trigger a nerve impulse which is seen as a brief flash of light. For most people the attachment of the vitreous to the retina is not particularly strong and these vitreous flashes and floaters are noticeable but not harmful. In a more severe case, the vitreous can pull the retina strongly and form a retinal tear or retinal detachment.
The retina is the nerve layer that lines the back of the eye and senses light with photoreceptors -rods and cones. The highest concentration of photoreceptors is located in the macula, the center of the retina. The macula is involved in the most sensitive, central and critical part of vision. Once light is sensed by photoreceptors, a nerve impulse is created. The nerve impulses are sent along retinal nerve fibers that bundle together to form the optic nerve. The optic nerve sends information that is received by the brain for visual processing and recognition. Due to the retina’s vital role in vision, damage to it can cause permanent blindness. If there is damage to the macula such as macular degeneration, your functional vision can really be severely impaired. If there is damage to the optic nerve, which is most commonly caused by an eye disease called glaucoma, your peripheral vision and eventually even your central vision can get progressively lost. A retinal detachment is another dangerous condition where part or all of the retina can be torn away. This can impair the retina from sensing light properly and sending visual information to the brain. Because there are so many sight-threatening retinal diseases, we highly recommend a thorough evaluation of the retina via means such as the Optomap Retinal Exam.